Infusion Providers Alliance
The Infusion Providers Alliance is a leading voice for in-office and freestanding ambulatory facility providers of drug infusion services. Alliance members are committed to preserving the integrity of the provider-patient relationship in a manner that delivers exceptional care to patients at a value to the health care system.
Our members have facilities located in communities across the nation, each of which offers a more convenient, more efficient and less expensive alternative for patients than receiving their infusions in the hospital setting. These facilities serve as critical access points of care for patients and save tremendous dollars for commercial and government payers alike while also lowering out of pocket costs for beneficiaries.
The Infusion Providers Alliance mission is to serve as a thought leader and to educate on issues critical to safeguarding, supporting, and strengthening provider directed, patient-focused access to in-office and freestanding ambulatory facility infusion services.
The Clinic-Based Approach Results in Substantial Savings and Better Outcomes
Administering infused and injected specialty drugs in the in-office or ambulatory infusion facility setting rather than the hospital setting can result in substantial prescription drug cost savings. In-office and freestanding ambulatory facilities can reduce administration costs of specialty medications by at least 50 percent for the top 10 HCPS codes—which account for approximately half of overall specialty medical spending–compared to the hospital setting.1,2,3 As a result, in 2017 and 2018 total drug costs were 5 to 7 percent lower than the hospital setting for Medicare patients, and one-third to two-thirds lower for Medicaid.4
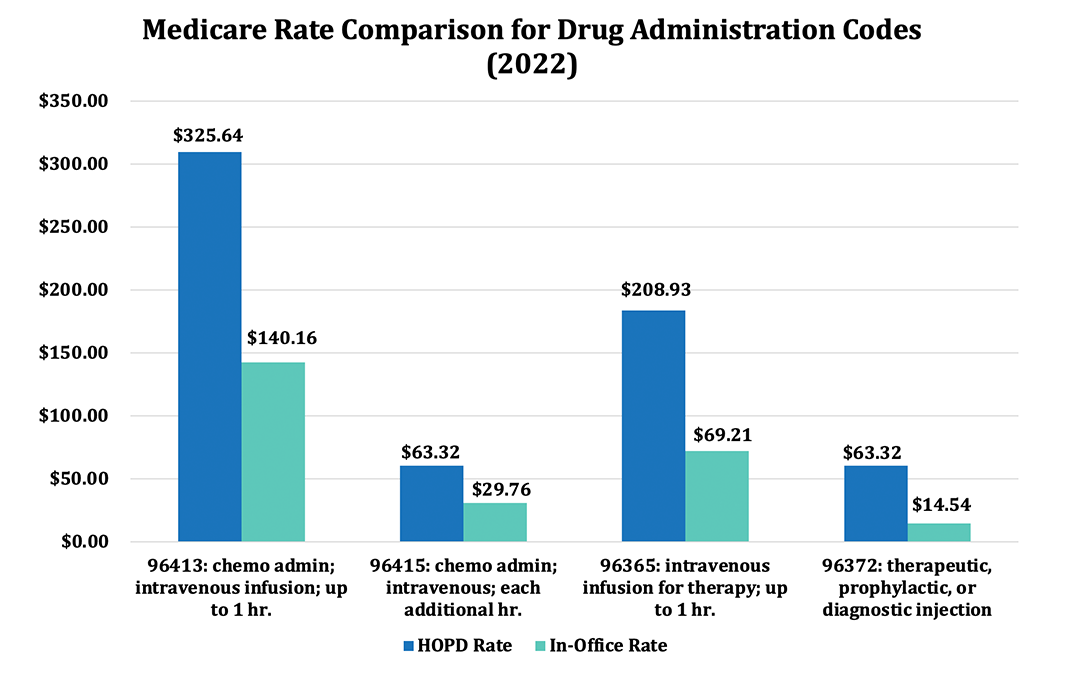
Medicare pays hospitals substantially more for infusion of identical drugs using identical staff time and skills as physician offices and freestanding ambulatory infusion centers, which are paid on the Physician Fee Schedule. For example, our infusion centers and practices regularly bill CPT code 96413 for the first hour of infusions of complex drugs such as Remicade, Ocrevus, and Entyvio for patients with a variety of diseases including Crohn’s disease, Multiple Sclerosis, and ulcerative colitis; for this particular CPT code, we are paid approximately 45 percent of the hospital rate: $309.56 vs $142.55. The payment differential widens more under CPT 96415 for additional hours of infusion: hospitals receive nearly double the physician office rate ($60.46 vs. $30.68). The contrast is even greater for CPT code 96372 for therapeutic, prophylactic or diagnostic injections such as for administering Boniva, Xolair, and Prolia for osteoporosis and arthritis: $60.46 in the hospital versus just $14.44 in the physician’s office, or 25 percent of the hospital cost.
Commercial payers also benefit from this more efficient delivery model. Infusions administered in hospitals can cost upwards to 3 to 5 times as much as infusions administered in in-office or freestanding ambulatory settings, yet more than half of routine infusions continue to be provided in hospital outpatient infusion centers. The UnitedHealth Group estimates that administering specialty drugs in the provider office or home instead of the hospital outpatient setting reduces the costs of drugs and their administration by $16,000 to $37,000 per privately-insured patient per year for the five conditions that account for nearly three-quarters of overall spending.5 The value and more efficient delivery provided by in-office or freestanding ambulatory infusion centers are also reflected in the commercial market—two-thirds of health plans have implemented site of care programs to drive down costs.6
Hospitals are also increasingly consolidating to leverage their market power for higher payment rates from commercial health plans. Evidence suggests that hospitals are financially incentivized by profits generated from the 340B program to consolidate and administer medicines in more expensive hospital outpatient settings.7 This often results in marked up provider-administered infusions and injections costs, which allow hospitals to receive payments from commercial health plans that are, on average, nearly 2.5 times the amount paid by the hospital to acquire the medicine. What is more troubling is that there is no clear evidence that consolidation improves the quality of care provided to patients. In fact, evidence has shown that hospital consolidation not only creates higher health care expenditures but causes negative health outcomes.8
Quality of Care
Physicians, nurses and highly trained medical personnel are better able to monitor a patient and ensure adherence if the infusions are done in an in-office setting. Office-based infusion services have been shown to produce improved patient adherence, a key metric for treatment of chronic and complex diseases that require infusions. A recent study by Stanford University found that patients receiving infusions in an office-based setting had a 79 percent adherence rate, compared to 74 percent at the hospital and 64 percent at home.9 Patients who received infusions at home were also 10 percent more likely to completely discontinue their treatment compared to patients who received infusions in an office-based setting (44.7 vs. 33.7 percent, respectively). Finally, patients who received infusions at home or at a hospital were less likely to visit their specialist for follow-up visits compared to patients who received infusions in an office-based setting. Patients who received infusions at home or a hospital visited their specialist on average 5 times and 4 times, respectively, while patients who received office-based infusions visited their specialist on average 14 times. Better drug adherence and increased monitoring through follow-up visits translates into better disease management.
In addition, patients enjoy a more relaxed atmosphere of the outpatient setting that prevents them from being unnecessarily exposed to severely ill and often contagious patients who need hospital care.
____________________________
- Bunger, Anna, Madeleine Cline, and Katie Holcomb. “Commercial Specialty Medication Research: 2019 Benchmark Projections.” Milliman. December 2019. https://www.milliman.com/en/insight/commercial-specialty-medication-research-2019-benchmark-projections
- Magellan Rx Management Medical Pharmacy Trend Report.” 2018. https://www1.magellanrx.com/documents/2019/03/medical-pharmacy-trend-report_2018.pdf
- “Magellan Rx Management Medical Pharmacy Trend Report.” 2019. https://issuu.com/magellanrx/docs/mptr2019?fr=sMmE2MTk0MDI3Nw
- “Magellan Rx Management Medical Pharmacy Trend Report.” 2018. https://www1.magellanrx.com/documents/2019/03/medical-pharmacy-trend-report_2018.pdf
- UnitedHealth Group, “Administering Specialty Drugs Outside Hospitals Can Improve Care and Reduce Costs by $4 Billion Each Year.” 2019. https://www.unitedhealthgroup.com/viewer.html?file=/content/dam/UHG/PDF/2019/UHG-Administered-Specialty-Drugs.pdf
- Magellan Rx Management, “Medical Pharmacy Trend Report.” 2019. https://www1.magellanrx.com/documents/2020/03/mrx-medical-pharmacy-trend-report-2019.pdf
- PHRMA, “Follow the Dollar Part II: Understanding the Cost of Brand Medicines Administered to Commercially Insured Patients in Hospital Outpatient Departments” February 2021. https://www.phrma.org/-/media/Project/PhRMA/PhRMA-Org/PhRMA-Org/PDF/0-9/2021-FTD-II-whitepaper_FINAL.pdf
- Kaiser Family Foundation, “What We Know About Provider Consolidation. September 2, 2020. https://www.kff.org/health-costs/issue-brief/what-we-know-about-provider-consolidation/
- Giese-Kim, May Wu, et al. “Home Infliximab Infusions are Associated with Suboptimal Outcomes Without Cost Savings in Inflammatory Bowel Disease.” The American Journal of Gastroenterology. July 22, 2020. https://journals.lww.com/ajg/Abstract/9000/Home_Infliximab_Infusions_Are_Associated_With.99217.aspx