Infusion Providers Alliance
The Infusion Providers Alliance is the leading voice for in-office and freestanding ambulatory facility providers of drug infusion services. Alliance members are committed to preserving the integrity of the provider-patient relationship in a manner that delivers exceptional care to patients at a value to the health care system.
Our members have facilities located in communities across the nation, each of which offers a more convenient, more efficient and less expensive alternative for patients than receiving their infusions in the hospital setting. These facilities serve as critical access points of care for patients and save tremendous dollars for commercial and government payers alike while also lowering out of pocket costs for beneficiaries.
The Infusion Providers Alliance mission is to serve as a thought leader and to educate on issues critical to safeguarding, supporting, and strengthening provider directed, patient-focused access to in-office and freestanding ambulatory facility infusion services.
The Value of “Buy and Bill”
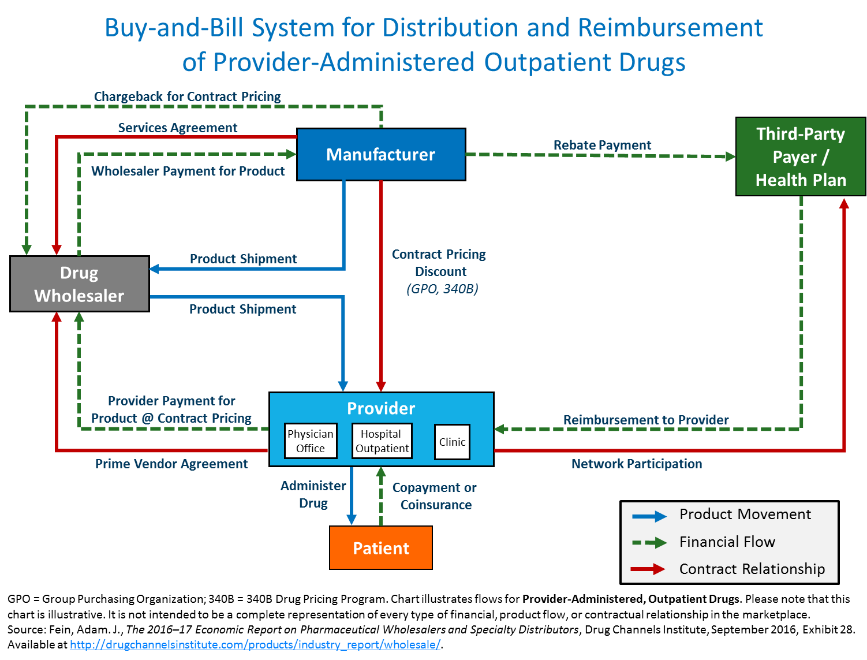
Infusion centers and provider offices rely on the current, well-established “buy-and-bill” distribution system that has provided uninterrupted and reliable patient access to Part B infused drugs for decades. Under “Buy-and-bill,” providers purchase and store Part B drugs and biologic medications in anticipation of administering these drugs to patients. This system gives providers control over the drug administration distribution and ability to manage drug inventory to ensure the appropriate medication will be on hand at the time of a patient’s visit.
Replacing the existing “buy-and-bill” model with a vendor-based model or PBM-controlled specialty pharmacy model will impair patient access to critical medications for patients with chronic conditions and place additional burden on the specialist provider community, many of whom have already suffered mightily due to the COVID-19 pandemic and resulting impact on their practice. These providers have kept patients out of the hospital setting, where they are more susceptible to COVID transmissions.
Operationally, replacing the “buy-and-bill” model creates other attendant issues. Oftentimes, a provider may change the dosing or other aspects of the drug regimen due to a change in a patient’s weight or lab value, and unless there is appropriate inventory on hand, the patient may not be able to receive their infusion at the required time, putting the patient at risk for a flare and subsequent hospitalization or other adverse outcome. In addition, a change to the model would lead to unnecessary wastage as the improper dosed vial cannot be used for other patients under a system that relies on patient specific orders. The buy-and-bill model permits providers to tailor the dose of medication for each patient prior to administration without fear of wasting pre-ordered medication by a vendor or pharmaceutical benefit manager. This substantially reduces cost to the healthcare system, particularly as total specialty medication costs continue to grow.
After administration, the provider submits a claim for reimbursement to Medicare or the appropriate commercial payor. For Medicare patients, providers are paid average sales price plus a small percentage This add-on payment accounts for variability in acquisition costs and ensures providers can properly recoup costs associated with shipping, storing, and administering these complex products.
Lastly, requiring the creation of a new supply chain adds a layer of cost to the provider community in the form of distribution fees that do not exist today with traditional wholesaler relationships. This additional expense would turn therapy administration from a low margin business to a money losing one, thereby causing providers to leave the market entirely, an outcome that would drive care back to most expensive setting, the hospital outpatient department, and create patient access issues as a result.
From 2006 to 2008, CMS experimented with a vendor-based distribution system under the “Competitive Acquisition Program.” That program failed for many of the reasons mentioned above and ultimately, only one vendor participated in the “competitive” program causing CMS to terminate the initiative.